You will be asked to perform emergent and urgent echocardiograms while on-call. General guideline is that only emergent and urgent echocardiograms be performed on off-hours. Ultimately, the decision regarding whether an echocardiogram is urgent or emergent will be based on clinical judgment. Sometimes, you will be requested to perform studies that you do not consider emergent or urgent. The attending on call can always be a resource in these cases although you will have to use clinical judgment and common sense.
Examples of potential emergencies that might warrant an echocardiogram:
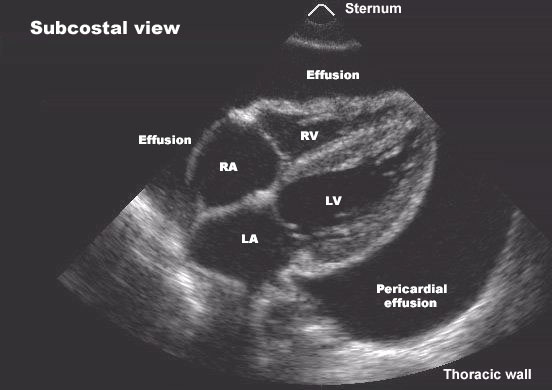
- Rule out tamponade (remember, a patient with normal BP, no pulsus, and a heart rate of 60 is not likely to be in tamponade). This is a common request on cardiac surgery service where tamponade may occur without a significant fluid collection due to extracardiac hematoma.
- Cardiogenic Shock: e.g. mechanical Complications of MI, trauma
- Hypotension of unclear etiology for which echo could be helpful
- Rule out aortic dissection (ascending): dissection/transection/rupture/intramural hematoma
- Assess RV function in a patient with suspected PE (debatable: an echo cannot rule out a PE).
Examples of requests that generally are NOT considered emergent
- Endocarditis, rule out vegetation (unless the patient is potentially a surgical candidate or this would change therapy)
- Assess LV function in a stable patient
- Routine pre-op
- Assess valvular function in a stable patient
- Rule out cardiac source of embolus
As a general rule, echos should only be performed at off-hours if the results of that study would markedly impact the patients’ care. When in doubt, or if your judgment is questioned by an attending physician, feel free to kick the issue up to the senior fellow or echocardiography attending on-call.
(From http://www.silkview.com/echo/BWHechocall.html)